- Show Menu
- Contact Us
- FAQs
- Reader Service
- Survey Data
- Survey Winners
- Testimonials
- Upcoming Events
- Webinars
- White Papers
Automating Chemotherapy Ordering and Administration
Brigham and Women’s Hospital (BWH) is a tertiary academic medical center affiliated with the Dana-Farber Cancer Institute. Of our 777 beds, 110 are used for hematology, oncology, and hematopoietic stem cell transplant patients. To help minimize potential medication errors with these patients, BWH rolled out a chemotherapy order entry (COE) system in 1997 that incorporates computerized provider order entry (CPOE) and pre-programmed templates for high-risk chemotherapy patients, including all hematopoietic stem cell transplant protocols. This system generates orders that are sent via an interface to our pharmacy system, and from there, the orders are approved, prepared, and sent to the nursing units for administration. When COE was first implemented, nurses used paper charts to document medication administration. By 2003, BWH began implementing an electronic medication administration record (eMAR) system with bar code medication administration (BCMA). The system was initially rolled out in general medicine, surgery, and the intensive care units. Because of the complex scheduling issues inherent to chemotherapy protocols and regimens, we held off on rolling out eMAR on the chemotherapy units until specific enhancements to the system were made.
Click here to view a larger version of this Figure
Chemotherapy eMAR Considerations
In 2005, a multidisciplinary team—composed of pharmacists, physicians, nurses, computer analysts, and computer programmers—was assembled to collaborate on developing an eMAR system for oncology patients. Developing an effective system meant reviewing and modifying many practices in place at the time. It also meant devising functions for the system to best support the new practices.
Some of the questions that needed to be answered before developing this system included:
- What is a chemotherapy day when compared to a calendar day?
- Who should be responsible for the timing and sequence of the chemotherapy and associated medications?
- Who should be allowed to change the time of the chemotherapy and the supportive care medications after approval?
Chemotherapy Day vs. Calendar Day
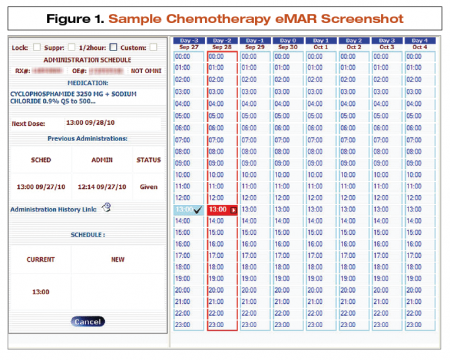
Before employing chemotherapy eMAR, orders were either interpreted as a calendar day or a chemotherapy day depending on the regimen and/or the time of day the chemotherapy started. As the new system would only support one definition, we needed to standardize how a day was defined. Considering many chemotherapy regimens are administered over the course of several consecutive days and are often started at different times during the day, we chose to use chemotherapy day, which is based on the start time of the chemotherapy administration. This allows for a full chemotherapy day to be scheduled over two partial calendar days, ensuring that regimens started mid-day that need to continue past the end of the calendar day will not be disrupted. After coordinating a start time with nursing, pharmacists electronically set the chemotherapy day, which runs on its own twenty-four-hour clock (see Figure 1). So, for an infusion starting at 3pm and running for 24 hours, chemotherapy day two begins at the end of the first infusion (ie, at 3pm on the second calendar day).
Medication Scheduling
We also reviewed and modified our chemotherapy and supporting medication-scheduling practices and developed functions in the system to help with the changes. Prior to chemotherapy eMAR implementation, physicians entered orders via COE and CPOE, which pharmacists then approved. Subsequently, it was the responsibility of nursing to map out the sequence of medication administrations on paper, and document them on a patient’s paper chart after administration. We decided to transfer scheduling responsibilities from nursing to pharmacy, and developed a scheduling function in the system that enables the pharmacist to map out the hydrations, pre-medications, and chemotherapy in order of administration on an electronic chemotherapy card. The eMAR system then prompts the nurse to administer the products.
To assist pharmacists with scheduling regimens we developed a linking function that ties certain medications together automatically. This way, once the pharmacist approves an order, all linked medications will appear at their default time on the chemotherapy scheduler. For example, the pre-medications for paclitaxel are pre-programmed thirty minutes prior to paclitaxel administration. Medications also can be linked through a mutually exclusive function; for a patient with intravenous and oral options of the same medication and same dose, the pharmacist can create an exclusive link. Thereby, when the nurse scans the oral option of a dose for administration, the intravenous option of the same drug cannot be administered until the next dose is due. A linking function also is used for mix-together products—chemotherapy medications combined together in the same delivery system for a single administration. For example, when preparing intrathecal chemotherapy, methotrexate, cytarabine, and hydrocortisone in one syringe for administration, the challenge was determining how to approve all three drugs in a single chemotherapy order and ensure that the eMAR system could mark all three medications as administered. By using the mix-together function, we can link all three products together in the system, and when the computer-generated bar code label on the product is scanned, the eMAR system checks all three products as administered.
Administration Time Changes
On top of giving pharmacists the responsibility of scheduling regimens, we also charged them with changing administration times for chemotherapy after approval. So, if a nurse is unable to administer chemotherapy at the specified time, they simply contact the pharmacist to adjust the schedule of all pre-medications and chemotherapy. A move-up chemotherapy functionality was developed for chemotherapy that needs to be administered earlier on day two than it was on day one.

Lessons Learned
In June 2009, we ran a pilot of the chemotherapy eMAR system on a single oncology unit. From that trial, areas of improvement were identified. For example, we realized whenever administration times were changed in the system a new label automatically printed for the medication, thus rendering the label already on the prepared product unscannable. This meant that the product had to be returned to the sterile products suite for relabeling prior to administration. To address this, a system update was installed that now enables the pharmacist to suppress the label-print function when there are time changes or order edits for products already sent to the floor—eliminating the need to relabel the bag.
In August 2009, full eMAR rollout began, and every two weeks, two nursing units went live with the system; the rollout lasted approximately three months. After going live with our chemotherapy eMAR system-wide, we realized additional improvements were needed. Of note, pharmacist workload increased due to the new scheduling function; not only was pharmacy now responsible for coordinating with nursing for the start time of chemotherapy, they also were responsible for setting up the entire sequence of pre-medications, hydrations, and chemotherapies. To assist with this increase in workload, we developed standard administration times for our hematopoietic stem cell transplant patients, who are typically admitted the night prior to starting chemotherapy. In doing so, we decreased the time needed for scheduling and planning of some of our chemotherapy orders.
We also changed our process for batching chemotherapy and developed a functionality to accommodate this process change after we discovered the force-print label function we used when preparing orders on demand was incompatible with the eMAR system. Our normal sterile products batch print takes place at the start of both the day shift (6am) and the evening shift (3pm). Prior to eMAR, chemotherapy was produced as part of the morning batch print with all of the other compounded sterile products and then as needed throughout the day; the force-print action we used to print labels for products that needed to be prepared on demand was not compatible with the dose counting functionality of eMAR, and the bar codes on the force-print labels would not scan at the time of administration. To address this, we decided to batch chemotherapy separately, and we created a batch print functionality for our chemotherapy products that enables our sterile products room pharmacist to print an on-demand chemotherapy batch; so, now chemotherapy can be batched at any point in the day. New start chemotherapy and chemotherapy products with short expiration dates are the only medications produced by the evening-shift pharmacists.
Conclusion
Despite the overall success of our chemotherapy eMAR, there are still areas at our institution where chemotherapy is administered without the use of this technology. Going forward, we hope to expand our chemotherapy eMAR capabilities to the operating room and interventional radiology in order to move closer to our goal of a seamless digital pathway from the physician’s order to medication administration throughout our entire institution.
 Anne McDonnell, PharmD, BCOP, is a clinical pharmacy specialist at Brigham and Women’s Hospital in Boston, Massachusetts, where she has worked for the past five years. She received a BS in pharmacy from Massachusetts College of Pharmacy and Health Sciences and a doctor of pharmacy from the University of Arkansas for Medical Sciences. She also completed a pharmacy practice residency program at New York-Presbyterian Hospital and an oncology pharmacy practice residency at the Medical University of South Carolina & College of Pharmacy.
Anne McDonnell, PharmD, BCOP, is a clinical pharmacy specialist at Brigham and Women’s Hospital in Boston, Massachusetts, where she has worked for the past five years. She received a BS in pharmacy from Massachusetts College of Pharmacy and Health Sciences and a doctor of pharmacy from the University of Arkansas for Medical Sciences. She also completed a pharmacy practice residency program at New York-Presbyterian Hospital and an oncology pharmacy practice residency at the Medical University of South Carolina & College of Pharmacy.
Like what you've read? Please log in or create a free account to enjoy more of what www.pppmag.com has to offer.








